Extending
1
View details
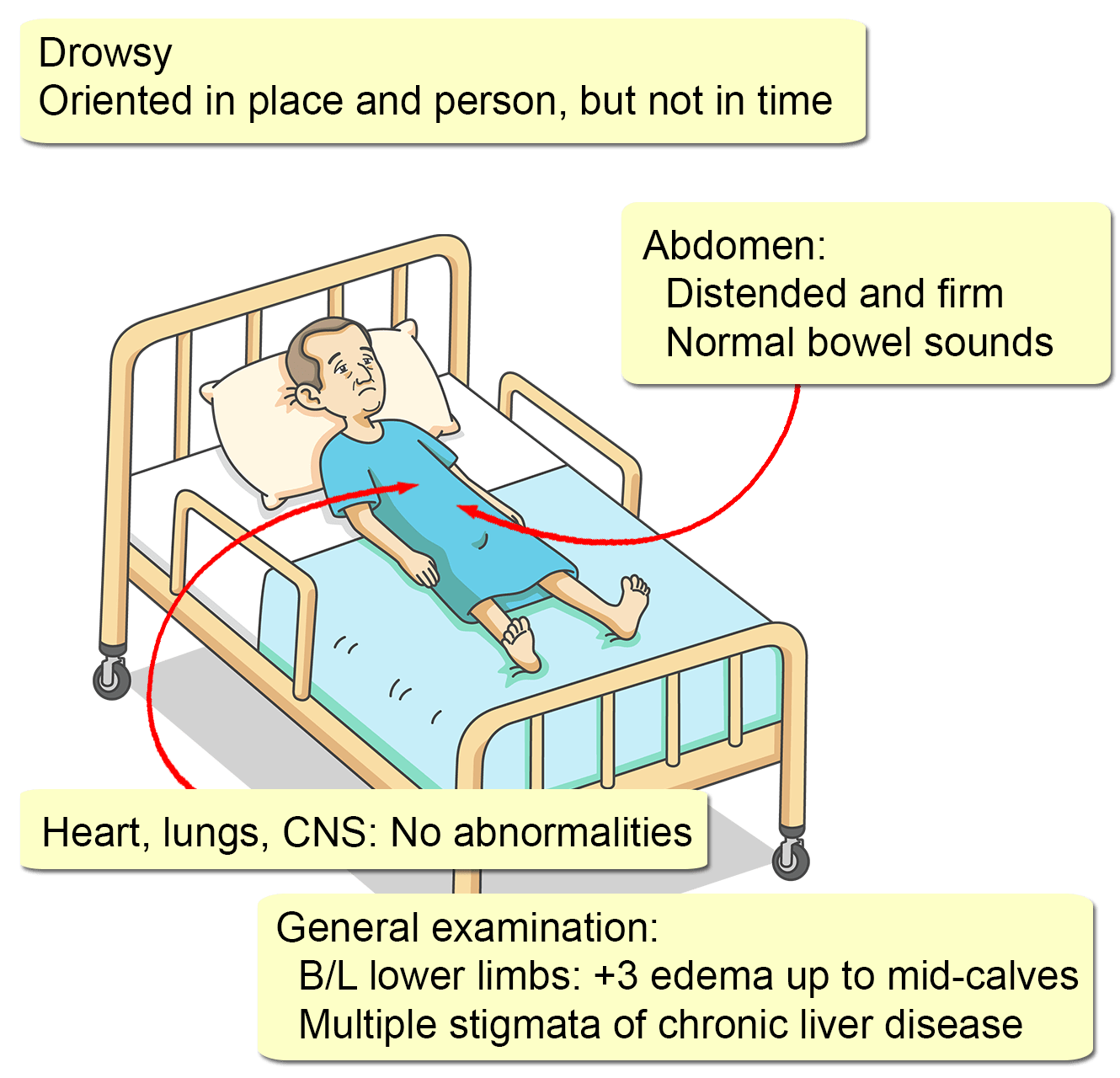
A 52-year-old Caucasian man presents with mild dyspnea, abdominal distension, bilateral leg swelling, and reduced urine output for four days. There was no history of fever, cough, wheezing, hematemesis, melena, or urinary or bowel symptoms.
He was diagnosed with end-stage liver disease (ESLD) due to alcohol abuse one year ago and is currently on the combination of furosemide, spironolactone, and propranolol. He has stopped drinking since the time of diagnosis but shows poor drug compliance.
His medical and surgical histories are otherwise unremarkable, and he is not on any other medications, including over-the-counter drugs, or herbal supplements. There are no known allergies.
His last clinic visit was approximately one week ago. At that time, his serum creatinine was 1.4 mg/dL (0.3-1.7).